By: Michael Verano, ICISF Member and Approved Instructor
As an Employee Assistance Program embedded in a large hospital system in Virginia, we are seeing first-hand how the trauma of Covid-19 is impacting health care workers. From 1:1 counseling sessions with nurses, techs and doctors, to consultations with leaders at all levels, the Corona Crisis is starting to wear away at the otherwise failsafe coping mechanisms of healthcare workers.
During times like these calls for critical incident responses take on a new form and present challenges to both those providing the service and those in need of individual crisis intervention, defusings or debriefings. In most cases the requests are, understandably, coming from hot zones of infection—ICUs running out of beds, the transformed ER now a quarantine zone, and from staff who are shuffled in and out of areas with high contact with contagious patients.
Requests for CIR teams in our area are focusing on addressing the issue of moral distress and moral injury being experienced by front line workers. Moral distress is defined as a form of stress experienced by individuals in response to an internal conflict between knowing what is needed and believed to be appropriate while, simultaneously, being unable to provide it due to constraints that are beyond their control. Healthcare workers are particularly vulnerable because their professional calling is rooted in the tenets to heal and do no harm.
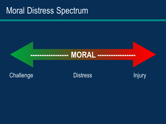
The spectrum of moral distress moves from the challenge zone, where most healthcare workers are operating these days, with moderate levels of stress, through distress where the toll begins to impact both professional and personal lives. The injury stage is where workers begins to question their usefulness and staying power and often consider leaving the field.
At Optima EAP, we have found it beneficial to make use of the full spectrum of CISM mechanisms to address these problems. We have encouraged hospital leaders to get out in front of their employees through crisis management briefings often staged as town hall meetings. During these meetings the topic of moral distress is discussed along with detailed plans for assisting the workforce in collaboration with other support services such as chaplaincy, EAP, internal CIR teams and a leadership institute to train managers on how to spot and address moral distress.
Due to the ongoing nature of this crisis and the uncertainty of when the next wave comes, we have found that using modified RITS and CISD models help to support those still on the front lines during their work shifts and to assist them in making a successful transition to home life. Handouts with multiple resources specific to moral distress are at the ready and distributed throughout the hospital. Finally, a script for an end of shift huddle was developed to encourage mangers to take the emotional temperatures of their staff and encourage focusing on positive accomplishments.
The modified debriefs are offered when a particular work group has completed an especially challenging shift and the manager has assessed the situation with the clinical supervisor associated with the peer team. The standard CISD model is utilized with the focus being the team’s combined experience with moral distress and to assess those who may be heading toward injury and need 1:1 attention. The group also has the opportunity to experience empathetic rounding, which unlike typical medical rounding, which focuses on patients, focuses on the well-being of healthcare workers in relation to their work with patients.
With no certain end if site, it is essential that CISM teams continue to grow and operate while remaining flexible in their approaches to meet the needs of those struggling to help and heal those exposed. There has never been a more important time for the introduction of peer support teams and a fully operational CISM model to ensure that moral injuries do not become the legacy of this pandemic.